What Really Impacts Your Blood Glucose (and How to Improve It)
Chrissie Kremer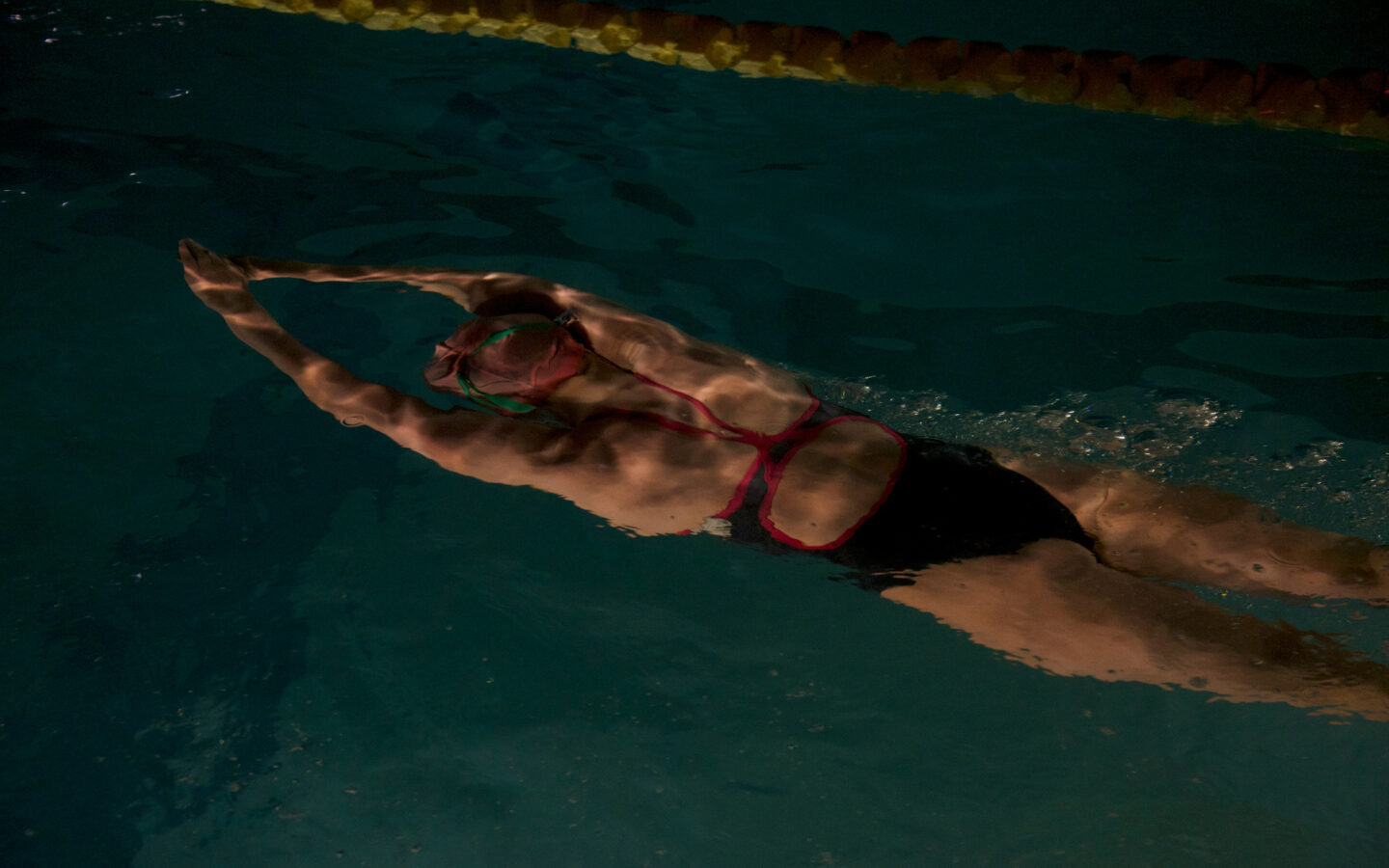
Glucose isn’t just about sugar. Discover the surprising factors that affect your blood sugar and 7 science-backed habits to improve your metabolic health.
When we think about blood sugar, we tend to picture desserts, soda, or that mid-afternoon crash after a carb-heavy lunch. But glucose, the body’s primary energy currency, isn’t just a dietary concern. It’s a central player in your metabolism, mood, cognition, energy, and long-term health. As we age, how efficiently we regulate glucose can influence everything from brain health and cardiovascular risk to [in-fluh-mey-shuhn]nounYour body’s response to an illness, injury or something that doesn’t belong in your body (like germs or toxic chemicals).Learn More, recovery, and [ri-zil-yuhns]nounThe ability to recover quickly from stress or setbacks.Learn More. In fact, many of the chronic conditions associated with aging, like type 2 diabetes, cognitive decline, and [hahrt dih-zeez]nounConditions affecting heart health and circulation.Learn More, are linked to unstable glucose levels long before symptoms appear.
The good news? Glucose regulation is highly modifiable. And thanks to new tools like over-the-counter continuous glucose monitors (CGMs), it’s easier than ever to track your blood sugar in real time and personalize your health strategy.
What Is Glucose?
Glucose is the body’s foundational fuel, essential not just for energy, but for nearly every function that keeps you alive and thriving. It powers your muscles, fuels your brain, supports cellular repair, and drives the production of ATP (the body’s energy currency). While carbohydrates and proteins ultimately break down into glucose, this simple sugar becomes a central player in metabolism, brain function, and hormone regulation.
Your body works hard to maintain glucose within a narrow optimal range. After a meal, blood sugar rises. In response, your pancreas releases insulin, which acts like a key, unlocking cells so glucose can enter and be used or stored. When blood sugar drops, your liver releases glucose back into circulation. This delicate feedback loop, governed by insulin and glucagon, is what keeps your energy stable.
But when this system begins to falter, due to chronic stress, poor sleep, excess belly fat, or [in-suh-lin ri-zis-tuhns]nounA condition where cells in the muscles, fat, and liver don’t respond properly to insulin, leading to impaired insulin sensitivity and potentially prediabetes or type 2 diabetes.Learn More, glucose regulation becomes less efficient. Over time, that inefficiency contributes to inflammation, fatigue, brain fog, and increased risk of metabolic disease.
Recent research shows that:
- Stable glucose decreases disease risk: Stable levels are associated with lower risk of type 2 diabetes, cardiovascular disease, and cognitive decline.
- Glocose metabolism is a whole-body effort: The liver, pancreas, muscles, adipose tissue, and even the nervous system all participate in glucose regulation.
- Early glucose disruptions are silent: Disruptions in glucose metabolism, even before diabetes is diagnosed, can silently damage blood vessels, impair hormonal rhythms, and interfere with energy production at the cellular level.
And here’s the nuance: glucose metabolism isn’t just about food. It’s also shaped by circadian rhythms, sleep quality, stress hormones like [kawr-tuh-sawl]nounA hormone that helps manage stress, energy, and alertness.Learn More, and even the [mahy-kroh-bahy-ohm]nounThe community of microorganisms (bacteria, viruses, fungi) living in a particular environment, especially the gut.Learn More. You can think of glucose as the body’s most tightly regulated fuel, and one of the clearest early signals of metabolic imbalance when things go awry.
How Can You Measure Your Glucose Levels?
The FDA approved an over-the-counter (OTC) Continuous Glucose Monitor (CGM), making real-time blood sugar tracking more accessible than ever. Originally designed for people with diabetes, CGMs are now gaining popularity among health-conscious individuals looking to optimize energy, metabolism, and [lon-jev-i-tee]nounLiving a long life; influenced by genetics, environment, and lifestyle.Learn More. Unlike traditional finger-prick tests, CGMs provide continuous insights into how food, exercise, and stress impact blood sugar levels—without requiring a prescription.
One of the biggest CGM insights? Glucose responses vary widely between individuals, even to the same meal. What sends one person’s glucose soaring may be perfectly stable for another.
What Can Impact Your Glucose Levels?
Most people associate glucose spikes with obvious dietary culprits: refined sugar, white bread, and ultra-processed snacks. And it’s true: what you eat, how much you eat, and when you eat are major players in glucose regulation. But those aren’t the only influences on your blood sugar. Glucose levels are shaped by a complex web of internal and external inputs, from hormones to hydration, stress to sleep.
Once you start tracking your glucose (with a CGM or simply through habit changes), you may be surprised by what throws you off balance. According to the Centers for Disease Control and Prevention (CDC), these lifestyle factors also play a role:
- Lack of Sleep: Poor sleep reduces [in-suh-lin sen-si-tiv-i-tee]nounHow effectively your body uses insulin, which regulates blood sugar levelsLearn More, making it harder for your body to regulate blood sugar.
- Caffeine Sensitivity: Some coffee drinkers experience blood sugar spikes in response to caffeine.
- Dehydration: Less water in your system means higher glucose concentration.
- Exercise Type: Some cardio workouts, like endurance running or HIIT, can initially spike blood sugar due to cortisol and glycogen release, while low-intensity movement like walking tends to lower glucose. [strength tray-ning]nounResistance-based exercise to build muscle and support healthy aging.Learn More may cause a short-term increase but improves glucose metabolism over time because muscle is a glucose sink.
- Skipping Breakfast: Frequently skipping breakfast can cause larger blood sugar spikes later in the day.
- Stress: Emotional and physical stress trigger cortisol, which raises blood sugar levels.
What to Know Before Tracking Your Glucose Levels
- It’s a Tool, Not a Solution: A CGM can provide useful insights, but sustainable metabolic health still comes down to whole-food nutrition, movement, and lifestyle habits.
- Food Responses Are Highly Individual: A CGM helps identify personal triggers, and what works for one person may not work for another.
- The Data Can Be Overwhelming: Some users report becoming overly cautious or anxious about food choices. Tracking should be a guide, not a source of stress.
If you’re curious about how your body responds to food, exercise, and stress, a CGM could be a valuable tool. But trends and patterns matter more than momentary spikes, sustainable habits like eating fiber-rich meals, managing stress, and strength training will always be the foundation of long-term health.
7 Simple Habits to Boost Glucose Sensitivity
- Strength Training
Resistance training improves insulin sensitivity by increasing [muh-suhl mas]nounThe total weight of muscle in your body, critical for longevity.Learn More, which serves as a glucose reservoir. A 2021 meta-analysis found that strength training significantly improves glucose control in men. - [zohn too kar-dee-oh]nounLow-intensity endurance training that builds metabolic health.Learn More
Low-to-moderate intensity cardio (like brisk walking, cycling, or swimming) improves mitochondrial efficiency and insulin signaling. A recent study found that 8 weeks of aerobic training improves glucose uptake and insulin action in women. - Post-Meal Walking
Walking for just 2 minutes or up to 30 minutes after meals reduces postprandial glucose spikes. Walking immediately after meals is more effective at lowering glucose levels than walking at a different time.
- Eat Protein and Fiber First
Eating protein and fiber before carbs slows glucose absorption and improves insulin response. In a 2023 study of adults with type 2 diabetes, eating vegetables and protein before carbohydrates led to a 73% lower post-meal glucose response compared to eating carbs first. - Eat More [pol-ee-fee-nawlz]nounPlant compounds that act as antioxidants.Learn More
Found in berries, dark chocolate, tea, and colorful plants, polyphenols reduce oxidative stress and improve glucose regulation. Polyphenols boost insulin sensitivity and endothelial function. - Get Consistent, High-Quality Sleep
Just 1–2 nights of poor sleep can cause insulin resistance even in healthy people. Aim for 7–9 hours. Partial sleep restriction impairs insulin sensitivity in healthy adults. - Manage Stress
Chronic cortisol release interferes with glucose metabolism. Practices like [breth-wurk]nounIntentional breathing exercises that reduce stress and improve focus.Learn More, meditation, or yoga help. [mahynd-fuhl-nis]nounThe practice of paying attention to the present moment with non-judgmental awareness.Learn More-based stress reduction improves glycemic control in adults with insulin resistance.
The information provided in this article is for educational and informational purposes only and is not intended as health, medical, or financial advice. Do not use this information to diagnose or treat any health condition. Always consult a qualified healthcare provider regarding any questions you may have about a medical condition or health objectives. Read our disclaimers.